Provider Education
Mississippi Division of Medicaid Advanced Imaging Preauthorization
Training Materials
DIVISION OF MEDICAID BREAKING NEWS
New Prior Authorization Provider Portal Available for Registration
As previously announced, the Mississippi Division of Medicaid (DOM) will transition to Telligen, a new Utilization Management/Quality Improvement Organization (UM/QIO), in early 2024.
To ensure you have adequate time to transition we ask that beginning December 1, 2023, providers begin registering with Telligen for the purpose of submitting prior authorization requests for Medicaid fee-for-service (FFS) members. Telligen will be the UM/QIO vendor to replace the following:
- Alliant Health Solutions ̶ responsible for medical authorization requests
- Kepro(formerly eQHealth Solutions) ̶ responsible for advanced imaging authorization requests
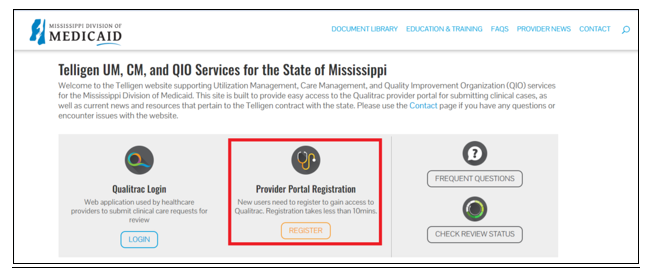
Providers are advised to visit Telligen’s Mississippi UM/QIO website beginning December 1, 2023 to register for portal access. Look for the Provider Portal Registration option, as indicated in the red box below. https://msmedicaid.telligen.com.
Please note: Prior authorizations for members enrolled in MississippiCAN and CHIP will continue to be handled by the respective coordinated care organization.
Training Calendar
MS Medicaid Advanced Diagnostic Imaging Provider Education Webinars
There are no webinars scheduled at this time. Please check back for future webinar schedules.
Education and Forms
Provider Manual and Quick Reference Guides
This manual should be used in conjunction with the MS Division of Medicaid's Administrative Code and Provider Billing Rules.
MS Advanced Diagnostic Imaging Provider Manual
Quick Reference Guides
How to Complete A Saved Request
How to Reset A Password or Unlock an Account
How to View a Determination Letter
How to Add Supporting Documentation
How to Make a Revision to a Submitted Review
Webinar Presentations
Prior Authorization Information
The Prior Authorization Form should only be used when access to the Atrezzo web portal is temporarily unavailable. Please contact 866 740 2221 if you are having difficulty logging into the portal.
Retrospective Authorization requests may be submitted using the Prior Authorization Request form when the Atrezzo web portal is temporarily unavailable.
Reconsiderations
When an adverse decision (denial based on medical necessity) has been made on a prior authorization request, the member or provider may request a Reconsideration within 30 days of the adverse determination letter. Please refer to the Advanced Imaging Provider Manual for more details. A reconsideration request CANNOT be made for Technical Denials.
This form should only be used when access to the Atrezzo web portal is temporarily unavailable.
Videos
MS ADI Provider Portal Create A Case Wizard
Questions and Answers
Accessing Atrezzo
First time Log in/Registration Instructions:
1. If you currently have a Kepro account for other lines of business, please email msadihelp@kepro.com with your name, phone number, Kepro username and NPI AND MS Medicaid number of the group you are needing access to. Kepro staff will provide access to the MS Medicaid contract under your established Kepro account. New registration is not required.
2. If your group has never used Kepro for other lines of business, the Provider Group Administrator will need to register the group or hospital NPI for the first time and create each user an account. A short tutorial video can be found in the Video section.

